Wednesday, 23 February 2022
Fused Glass Project Sheet
Sunday, 20 February 2022
Enhancing Road Marking Paints using Spherical Glass Beads
Enhancing Road Marking Paints using Spherical Glass Beads
Posted Krista Grayson on Aug 7, 2018

Road markings make a vital contribution to road safety and optimizing use of road space and make it possible to provide information that it is not easy to convey using mounted signs.1 Furthermore, signage applied directly to the road surface provides a form of continuous messaging which can be seen when a verge-mounted sign may be obscured.
The effectiveness of road markings in enhancing the safety of road users depends on the markings being clearly visible. This becomes particularly important at times of low light, such as during night time, rain or fog. Since the visibility of road markings is a crucial factor in ensuring traffic safety, strict performance requirements have been introduced to ensure the efficacy of road markings, which must be checked and maintained on a regular basis. European reflectivity standards (European Standard EN 1436) stipulate the minimum levels of daytime and night-time visibility as well as color and skid resistance.3
Road markings come in a range of formats, including thermoplastic, screed, spray, extrusion and ribline, but all must meet strict visibility requirements.
Improving the Visibility of Road Markings
Recent collaborative European research has determined the minimum distance at which road markings should be visible to drivers to be equivalent to two seconds of travel time.5 The distance from which a road marking is visible depends on a variety of factors.4,5 Many of these are driver-related, e.g., the driver’s vision, car cleanliness, headlight strength; or unavoidable, e.g., glare from oncoming vehicles, rain. The composition of the road marking however can be designed to optimize its visibility in a range of conditions. For example, titanium dioxide pigment is used to maintain the bright color of road markings and crystallized titanium dioxide is added to prevent the build-up of dirt on markings, which would reduce their visibility.
Most of the light emitted by the headlights which hits the road surface is reflected forwards or absorbed by the road surface itself with only a fraction of the light reflected back towards the driver’s eyes. The reflecting of light back in the direction of the light source is known as retroreflection.5,6 The higher the coefficient of retroreflected luminance the greater the contrast between the road marking and the road surface. The more of the light from the headlights that a road marking reflects back to the driver, the more visible the road marking will be, especially at night and in bad weather.
Titanium dioxide and other such additives do not create retroreflection to enhance the luminescence of road markings. In contrast, the addition of glass beads increases retroreflection, whereby improving the night-time visibility of road markings. The headlight beam penetrates the glass bead, hits the pigmented road marking, and is reflected back towards the car driver. The road marking therefore appears to light up and so the visibility of the road marking is increased significantly. Road markings incorporating high performance glass beads are five times brighter than road markings that do not.
The extent of retroreflection achieved by glass beads depends on the size of the beads and the quality of the glass. The level of retroreflectivity is determined using the 30-metre geometry. This is the amount of reflected luminescence at an illumination distance of 30 m, a driver height of 1.2 m, and a headlamp height of 0.65 m.7 A minimum retroreflectivity of 120 mcd/m2/ lux on a dry surface is recommended.
Glass Beads – Road Marking Enhancement
Glass beads for use in road markings typically have a refractive index of between 1.5 and 1.9. They are produced in a variety of sizes ranging from 100 to 1500 microns in diameter and with varying degrees of roundness. Glass beads can be mixed into the road marking material during production (intermix beads), added as the road marking is applied (injection beads) or applied to the surface of newly applied road markings before they have set (drop-on beads).
The beads must be embedded by at least 50% of their diameter to ensure that they do not become dislodged. However, increasing the degree of bead embedment reduces the level of retroreflectivity, so an effective balance needs to be achieved. It is inevitable that some of the beads will become covered with the marking material but this will soon be rubbed off by passing traffic.
The quality of the retroreflection produced by the glass beads also depends on the size and roundness of the beads, the amount of beads added to the road marking and the viscosity of the road marking material. Highest retroreflective performance is achieved using the larger beads with smoother, more round surfaces. An effective distribution level of glass beads is 400 to 600 grams per square meter of road marking.
Mo-Sci Corporation produces glass spheres for a wide range of applications.8 Mo-Sci supplies high quality glass, which can be customized to meet specific project requirements. They produce glass beads suitable for increasing the visibility of road markings to tight specifications that guarantee optimum reflectivity.
Conclusion
Road markings are an essential safety feature. Glass beads significantly increase the reflectivity of paints on the road, which in turn significantly improves their visibility and consequently driver and pedestrian safety.
Glass beads are the only road marking additive that causes retroreflection, sending more of the headlight beam back to the driver. Consequently, glass beads make road markings at night time appear five times brighter than road markings that do not contain glass beads.
References & Further Reading
- Department of transport UK 2003. Traffic signs manual Chapter 5 Road markings. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/223667/traffic-signs-manual-chapter-05.pdf
- Charlton SG, et al. Using road markings as a continuous cue for speed choice. Accid Anal Prev. 2018;117:288?297. doi: 10.1016/j.aap.2018.04.029. Epub 2018 May 9.
- Highways Markings. A Guide to IS EN 1436 European Standard for Road Markings. Available at http://www.highwaymarkings.ie/documents/is_en_1436_1.pdf
- Owens Da, et al. Effects of age and illumination on night driving: a road test. Hum Factors 2007;49(6):1115?1131.
- The National Cooperative Highway Research Program. Chapter 3. Available at http://onlinepubs.trb.org/onlinepubs/nchrp/nchrp_syn_306_22-37.pdf
- Stoudt MD, Vedam K. Retroreflection from spherical glass beads in highway pavement markings. 1: Specular reflection. Applied Optics 1978;17:1855?1858.
- Pike AM, et al. Evaluation of Retroreflectivity Measurement Techniques for Profiled and Rumble Stripe Pavement Markings. Transportation Research Record 2011. Paper 11-1293. Available at http://docs.trb.org/prp/11-1293.pdf
- Mo-Sci Corporation. Company website available at http://www.mo-sci.com
Wednesday, 16 February 2022
Never refuse to refuse?
Sunday, 13 February 2022
Using Porous Glass Microspheres for Targeted Drug Delivery
Using Porous Glass Microspheres for Targeted Drug Delivery
Posted Krista Grayson on Jun 19, 2018
 Share
Share Tweet
Tweet Share
Share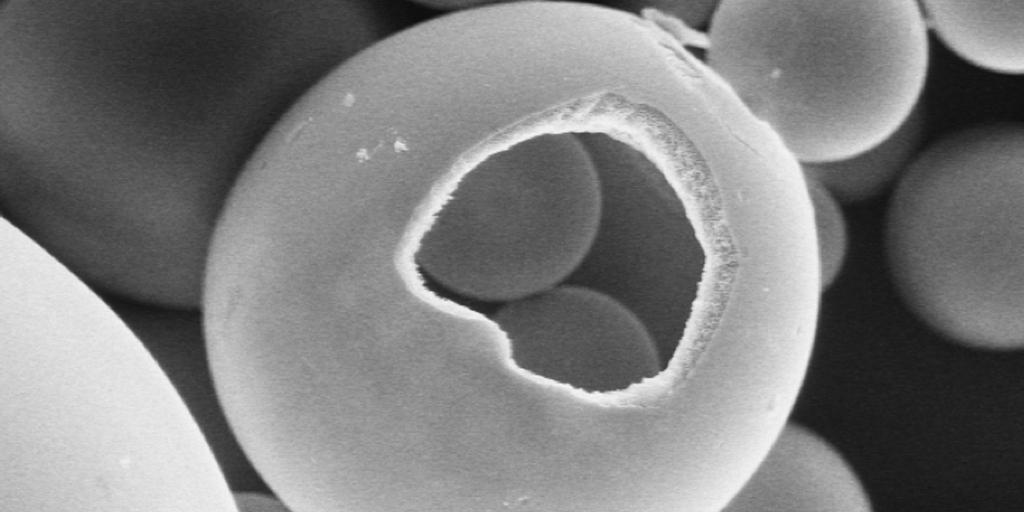
Finding methods for improving efficiency and bioavailability is central to targeted drug delivery. While controlled release dosage medication forms are the norm, they can encounter many limitations. One disadvantage is the difficulty of locating and retaining the drug delivery system within the gastrointestinal (GI) tract due to gastric emptying variation.1 This can cause drug release that is insufficient for the patient or result in shorter residence time of the dosage in the stomach.
To increase gastric retention and improve drug absorption, hollow microspheres have been developed and applied in the clinical setting for certain patients.2 Porous-wall hollow glass microspheres used in medicine are often produced from biopolymers, ceramics, bioactive glasses, and silicates. Hollow microspheres feature a 10 to 100 micron-diameter hollow cavity for the containment of certain substances.3
The most predominant mode for drug administration to the systemic circulation is the oral route. Some drugs have difficulty absorbing through the GI tract when using this route, prompting professionals to seek alternative methods for delivering pharmacologically active substances to the body.
The porous or hollow features of microspheres offer the ability to encapsulate fragile drugs and provides protection from biological compounds that may interfere with drug availability.4 These spherical, empty particles can remain in the gastric region for long periods of time and extend residence time of drugs in the GI tract.
Porosity offers improved loading efficiency and helps control the release of medications. Overall, hollow microspheres improve bioavailability of a drug, thereby reducing drug waste.
Microspheres can be produced to feature a uniform shape and size that can improve delivery of spheres to a specific target site. Additionally, microspheres are an ideal candidate for carriers of therapeutic agents due to their porosity, large surface area, and volume.
The hollow center of the microspheres reduces their density to such a degree that they have the potential to be buoyant. This behavior makes hollow microspheres suitable for use in a wide variety of applications.
Advantages of Porous Glass Microspheres
Hollow microspheres can reduce dosing frequency, allowing for improved patient compliance. Also, a desirable plasma concentration of a therapeutic agent can be maintained with microspheres by continuous drug release. The structure of the microspheres also results in an increase in gastric retention time, meaning therapeutic agents are released over a longer time. Other advantages of hollow microspheres include:
- Site-specific drug delivery to the stomach
- Sustained release effect helps avoid gastric irritation
- Short half-life drugs can achieve a better therapeutic effect
Limitations of Porous Glass Microspheres
Patients are required to consume a large amount of water for hollow microspheres to float and function. Instead of merely taking a sip of water with a drug (typical of the oral route of medication administration), patients must drink a full glass (200 to 250 ml) of water with the microsphere. In addition, hollow microspheres are unsuitable for drugs that feature stability and solubility issues in gastric fluids.
Savannah River National Lab (SRNL) and Mo-Sci Microspheres
The SRNL has teamed with Mo-Sci Corporation, experts in the production of specialty glasses, to create porous wall, hollow glass microspheres that consists of glass “microballoons” smaller than the diameter of a human hair.
SRNL’s microspheres feature a unique network of interconnected pores in the walls. These pores allow tiny “microballoons” to be filled with gasses as well as other materials. Each SRNL microsphere is around 50 microns in diameter, and the walls are around 10,000 angstroms thick. The walls feature pores that come to about 100 to 300 angstroms. Each pore allows gasses to entire the spheres and be stored or cycled on absorbents.
The original use for SRNL’s microspheres was to provide a solid-state storage method for hydrogen. Further research, however, has revealed their powerful utility and practical application in medicine. Currently, Mo-Sci plans to offer SRNL’s porous-walled hollow glass microspheres as a transport system for targeted drug delivery, among other uses.
Microspheres are being further investigated in an effort to discover new applications within healthcare. While further study is ongoing, microspheres will hopefully provide enhanced patient care and improve the effectiveness of medication delivery across a broad range of disease states.
References
- Kurrey A, Suresh PK, Singh MR. Hollow microspheres as a drug carrier: An overview of fabrication and in vivo characterization techniques. Chronicles of Young Scientists. 2014;5(1):1-10.
- Qing W, Wenhai H, Deping W. Preparation of hollow porous HAP microspheres as drug delivery vehicles. Journal of Wuhan University of Technology-Mater. Sci. 2007;22(1):174177.
- Hossain KMZ, Patel U, Ahmed I. Development of microspheres for biomedical applications: a review. Progress in Biomaterials. 2015;4(1):1-19.
- Li S, Nguyen L, Xiong H. Porous-wall hollow glass microspheres as novel potential nanocarriers for biomedical applications. Nanomedicine. 2010;6(1):127–136.
- Wicks GG, Heung LK and Schumacher RF. Microspheres and Microworlds. American Ceramic Society Bulletin, Vol. 87, No. 6
- http://www.mo-sci.com/porous-silica/
Wednesday, 9 February 2022
Frosting on slumped glass
[We’re] Having a few challenges with a stainless-steel S-curve mould (15cm x 10cm [prepared with boron nitride]. … When we slump a piece of glass, we get a frosted effect … in places where the glass was touching the mould at the beginning. I don't think it's devitrification, because the glass itself isn't cloudy, it's just hundreds of little bumps and dimples.
 |
| Photo credit: Adrian Cresswell |
This is a mould that combines draping and slumping in the
same firing. The glass must drape over the hump and slump into the valley at
the same time. This is effectively two processes in the same firing. It does
require some compromise in scheduling as a result.
It is of course possible that insufficient boron nitride was placed on the steel and the glass grabbed the steel. It is worth checking, although I don’t think it likely.
A summary
These stretch marks occur when the glass moves excessively against the mould. This
is usually a combination of high temperature and fast ramp rates. Slumping
should be done at the lowest practical temperature. The soak should be long,
rather than brief.
The Remedy
Fire more slowly and to a lower temperature. The Bullseye suggestion from their quick tips is for a double curve (or wave) mould of 250 x 210 x 40 mm (9.85" x 8.25" x 1.6"). They suggest a ramp rate of 167°C to 660°C /1221°F with a soak of 10 minutes for a 6mm/0.25” thick piece.
With gentle heating -slow ramp rate, long soak - the glass gradually conforms to the shape of the mould without stretching over the hump/crest of the mould. Instead, what happens is that the glass slips slightly from the opposite end of the mould. To counteract this, I place the glass 6mm/0.25” over the upraised end of the ceramic mould. This then finishes just inside the mould’s edge.
Low Temperature Kilnforming; an Evidence-Based Approach to Scheduling
Fitting Glass in Leading
Sunday, 6 February 2022
Bioactive Glass as a Bone Graft Substitute
Bioactive Glass as a Bone Graft Substitute
Posted Krista Grayson on May 16, 2018

Between 1992 and 2007, bone grafting was used in the treatment of almost two million patients in the United States.1 Bone grafts are used to facilitate the healing of complex bone trauma. This may be a multiple fracture or non-union of a long bone fracture, loss of bone due to disease, or surgical implantation of devices, like joint replacements, plates, or screws.
Bone grafting typically uses bone from another part of the patient’s body, such as ribs, hips, or pelvis, (an autograft) or bone harvested from a deceased donor or a cadaver that has been cleaned and stored in a tissue bank (an allograft).
Despite grafting markedly improving bone regeneration and clinical outcomes after severe bone injury or loss, there is still room for improvement. Researchers continue to investigate ways to enhance bone grafting techniques and provide faster and denser bone regeneration with lower morbidity.
One such development has been the use of bone graft substitutes, such as demineralized bone matrix, calcium phosphates, collagen- /hydroxyapatite-based substitutes, and bone morphogenetic proteins. Although autologous bone grafting was considered to be the preferred bone grafting modality,2 there is a trend towards favoring artificial bone grafts over autografts since they are readily available and obviate the need for additional surgery. However, bone graft substitutes can have limitations regarding strength under torsion.
Bioactive glass, by virtue of its biocompatibility, strength and range of achievable properties, has been widely used to facilitate bone repair and provide support in tissue engineering.3
The Different Types of Bone Grafting
Bone grafting is a surgical procedure that is beneficial for repairing bones that have been severely damaged by trauma and for replacing bone that is missing as a result of either trauma or disease. It can also be used to strengthen bone at the site of an implant, be that a joint replacement, screw or dental implant. The bone graft provides a framework to support and encourage the growth of new, living bone.
Autografts have long been considered the preferred means of bone grafting since they do not carry the risk of rejection. However, these necessitate additional surgery, which increases patient morbidity and the risk of infection. Furthermore, there may be issues with availability finding a suitable site to harvest bone of the needed shape and size.
Allografts obviate the need for additional incisions but carry the risk of immune response preventing the graft from being accepted. There is also still the potential for availability issues since the donated bone needs to be tissue matched with the patient.
A third option is not to rely on bone at all for the graft, but instead to use a man-made substitute. A range of different materials, including calcium phosphates, collagen, hydroxyapatite, have been investigated for use in bone grafting and are readily available. When using bone substitutes the nature of the materials must be carefully considered in terms of biocompatibility, resorption rate and strength.
Bone Graft Substitutes
The formation of new bone requires three key processes: osteogenesis (synthesis of new bone), osteoinduction (recruitment of stem cells and their differentiation into bone cells), and osteoconduction (the development of adequate blood supply to the new bone and correct structuring of the new bone cells). Bone graft substitutes are designed to facilitate and enhance these processes to promote rapid development of strong new bone.
Bone graft substitutes are frequently used to fill bone defects after orthopedic trauma. Ideally a synthetic bone graft substitute would have efficacy at least comparable to autograft, no immunogenicity, osteoinductive and osteoconductive properties, predictable resorption/degradation time, and no safety concerns.
Numerous studies have reported benefits of using synthetic bone substitutes for fracture treatment and spinal surgery.4,5,6,7 These include reduced pain, bleeding and healing time, and improved functional outcomes compared with autografts. However, there have been safety concerns and problems with unpredictable resorption rates with some of the bone substitute materials.8
Furthermore, the different bone substitute products have varying characteristics. They all only provide minimal structural integrity and none targets all three of the key bone formation processes.9 Although some bone substitutes closely mimic the structure of natural bone, they lack osteogenic and osteoinductive properties.
Bioactive glass has been successfully used in a range of tissue engineering procedures.3 With its versatility, achieved through the tailoring of properties through composition adjustments, its intrinsic strength and biocompatibility, bioactive glass was considered a prime candidate for improving synthetic bone substitutes.
Bioactive Glass for Bone Grafting
Introduction of bioactive glass into the body induces specific biological activity that causes soluble ionic species to be released. These lead to the glass becoming coated with a substance similar to hydroxyapatite. The formation of this layer allows bioactive glass to bond firmly with both hard and soft tissues. Furthermore, bioactive glass can be manufactured to release nutrients required for bone regeneration.
It has been shown that damaged bone regained its original strength more quickly when repaired using composite combined with bioactive glass compared with bone repair using composite alone and that the efficacy achieved is comparable to that of autologous bone grafting.10,11
A recent study compared spine fusion in rabbits using a mineralized collagen bone substitute with and without added bioactive glass. The bioactive glass-collagen composite was shown to closely mirror repair by autograft in terms of the amount and quality of the new bone.12 In addition, fusion occurred earlier when the collagen composite was augmented with bioactive glass.13
Conclusion
Bone grafting is an important tool for the repair of damaged or disease bone. The gold standard is autografting, which uses bone harvested from the patient to avoid rejection reactions. However, the increased morbidity caused by the additional surgery needed to acquire bone for grafting has resulted in an on-going quest to find an alternative. Bone substitutes have shown efficacy, but do not promote the formation of new bone. Bioactive glass is biocompatible and enhances strong new bone creation. Studies have now shown that the addition of bioactive glass to bone substitutes can increase their efficacy and bone healing characteristics to rival those achieved with autografting.
Mo-Sci produces medical implant grade bioactive glass in a form suitable for mixing with bone composites and can tailor its composition to meet specific requirements.13
References
- Kinaci A, et al. Trends in Bone Graft Use in the United States. Orthopedics 2014;37(9):e783 e788.
- Flierl MA, Outcomes and complication rates of different bone grafting modalities in long bone fracture nonunions: a retrospective cohort study in 182 patients. J Orthop Surg Res. 2013;8:33.
- Rahaman MN, et al. Bioactive glass in tissue engineering. Acta Biomaterialia 2011;7:2355 2373.
- Bajammal SS, et al. The use of calcium phosphate bone cement in fracture treatment: a meta-analysis of randomized trials. J Bone Joint Surg [Am] 2008;90-A:1186-1196.
- Swiontkowski MF, et al. Recombinant human bone morphogenetic protein-2 in open tibial fractures: a subgroup analysis of data combined from two prospective randomized studies. J Bone Joint Surg [Am] 2006;88-A:1258 1265.
- Lerner T, et al. A level-1 pilot study to evaluate of ultraporous beta-tricalcium phosphate as a graft extender in the posterior correction of adolescent idiopathic scoliosis. Eur Spine J 2009;18:170-9.
- Dimar JR, et al. Clinical and radiographic analysis of an optimized rhBMP-2 formulation as an autograft replacement in posterolateral lumbar spine arthrodesis. J Bone Joint Surg [Am] 2009;91-A:137 186.
- Carragee EJ, et al. A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. Spine J 2011;11:471 191.
- American Academy of Orthopaedic Surgeons. Bone-grafts: Facts Fictions and Applications. Presented at 70th Annual General Meeting. Louisiana 2003. Available at https://www.aaos.org/research/committee/biologic/bi_se_2003-1.pdf
- Havener MB, et al. Improvements in Healing with a Bioactive Bone Graft Substitute in a Canine Metaphyseal Defect. Poster at 55th Annual Meeting of the Orthopaedic Research Society. February 22–25, 2009
- Jia W, et al. Bioactive Glass for Large Bone Repair. Adv Health Mater. 2015;4(18):2842 2848.
- Pugely AJ, et al. Influence of 45S5 Bioactive Glass in A Standard Calcium Phosphate Collagen Bone Graft Substitute on the Posterolateral Fusion of Rabbit Spine. Iowa Orthop J. 2017; 37: 193–198.
- Mo Sci Corporation website. http://www.mo-sci.com/en/products
Wednesday, 2 February 2022
Firing different glass at the same time
Can I fire COE 90 and 96 in the same firing using the same schedule?
“Can I fire
different glasses in the kiln at the same time?”
Finding the
slumping temperature is determined less from the manufacturer than by
observation. This post tells you how to find the slumping temperature.
Getting Relevant People to Your Website
- Holidays
- Celebrations
- Awareness days and weeks (Mother’s Day, birdwatch month, Gardening week, etc).
These need to be detailed in specific terms to bring people who are buying for birthdays, aniverseries, weddings, etc.
- Windows,
- Kitchens,
- Decorative,
- Functional,
- Garden
Again, these need to be described in specific terms, e.g., splashbacks, dinner sets, wall art, etc.
But it is not only your own site that you need to promote. In promoting other sites that you are associated with, you spread the knowledge of what you do. By linking and liking sites or businesses that have been useful to you, you may also get reciprocal mentions. These all spread knowledge of what you do to a wider audience.
- Keep track of the questions you are asked at craft and trade fairs and use them.
- Use the questions you have of other crafts and craft workers, adjusted for your own work.
- You can develop questions by googling for answers to your own questions and see how they are phrased. Then use that kind of approach in outlining responses to the questions.