Bioactive Glass as a Bone Graft Substitute
Posted on May 16, 2018

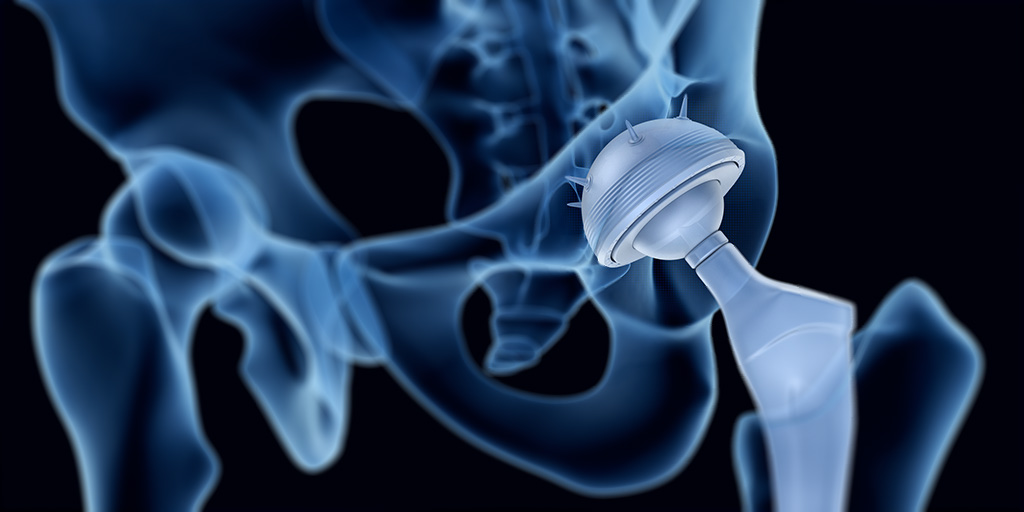
Between 1992 and 2007, bone grafting was used in the treatment of almost two million patients in the United States.1 Bone grafts are used to facilitate the healing of complex bone trauma. This may be a multiple fracture or non-union of a long bone fracture, loss of bone due to disease, or surgical implantation of devices, like joint replacements, plates, or screws.
Bone grafting typically uses bone from another part of the patient’s body, such as ribs, hips, or pelvis, (an autograft) or bone harvested from a deceased donor or a cadaver that has been cleaned and stored in a tissue bank (an allograft).
Despite grafting markedly improving bone regeneration and clinical outcomes after severe bone injury or loss, there is still room for improvement. Researchers continue to investigate ways to enhance bone grafting techniques and provide faster and denser bone regeneration with lower morbidity.
One such development has been the use of bone graft substitutes, such as demineralized bone matrix, calcium phosphates, collagen- /hydroxyapatite-based substitutes, and bone morphogenetic proteins. Although autologous bone grafting was considered to be the preferred bone grafting modality,2 there is a trend towards favoring artificial bone grafts over autografts since they are readily available and obviate the need for additional surgery. However, bone graft substitutes can have limitations regarding strength under torsion.
Bioactive glass, by virtue of its biocompatibility, strength and range of achievable properties, has been widely used to facilitate bone repair and provide support in tissue engineering.3
The Different Types of Bone Grafting
Bone grafting is a surgical procedure that is beneficial for repairing bones that have been severely damaged by trauma and for replacing bone that is missing as a result of either trauma or disease. It can also be used to strengthen bone at the site of an implant, be that a joint replacement, screw or dental implant. The bone graft provides a framework to support and encourage the growth of new, living bone.
Autografts have long been considered the preferred means of bone grafting since they do not carry the risk of rejection. However, these necessitate additional surgery, which increases patient morbidity and the risk of infection. Furthermore, there may be issues with availability finding a suitable site to harvest bone of the needed shape and size.
Allografts obviate the need for additional incisions but carry the risk of immune response preventing the graft from being accepted. There is also still the potential for availability issues since the donated bone needs to be tissue matched with the patient.
A third option is not to rely on bone at all for the graft, but instead to use a man-made substitute. A range of different materials, including calcium phosphates, collagen, hydroxyapatite, have been investigated for use in bone grafting and are readily available. When using bone substitutes the nature of the materials must be carefully considered in terms of biocompatibility, resorption rate and strength.
Bone Graft Substitutes
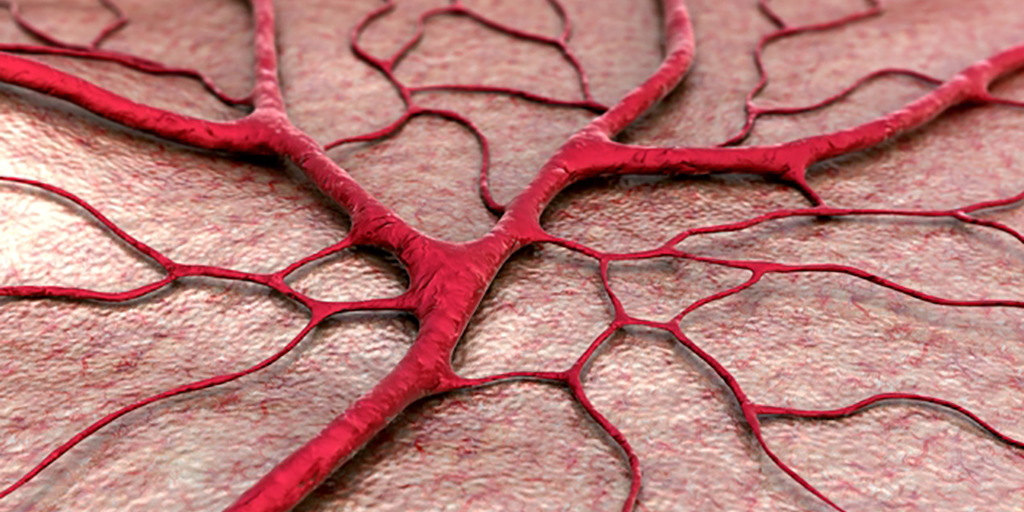
The formation of new bone requires three key processes: osteogenesis (synthesis of new bone), osteoinduction (recruitment of stem cells and their differentiation into bone cells), and osteoconduction (the development of adequate blood supply to the new bone and correct structuring of the new bone cells). Bone graft substitutes are designed to facilitate and enhance these processes to promote rapid development of strong new bone.
Bone graft substitutes are frequently used to fill bone defects after orthopedic trauma. Ideally a synthetic bone graft substitute would have efficacy at least comparable to autograft, no immunogenicity, osteoinductive and osteoconductive properties, predictable resorption/degradation time, and no safety concerns.
Numerous studies have reported benefits of using synthetic bone substitutes for fracture treatment and spinal surgery.4,5,6,7 These include reduced pain, bleeding and healing time, and improved functional outcomes compared with autografts. However, there have been safety concerns and problems with unpredictable resorption rates with some of the bone substitute materials.8
Furthermore, the different bone substitute products have varying characteristics. They all only provide minimal structural integrity and none targets all three of the key bone formation processes.9 Although some bone substitutes closely mimic the structure of natural bone, they lack osteogenic and osteoinductive properties.
Bioactive glass has been successfully used in a range of tissue engineering procedures.3 With its versatility, achieved through the tailoring of properties through composition adjustments, its intrinsic strength and biocompatibility, bioactive glass was considered a prime candidate for improving synthetic bone substitutes.
Bioactive Glass for Bone Grafting
Introduction of bioactive glass into the body induces specific biological activity that causes soluble ionic species to be released. These lead to the glass becoming coated with a substance similar to hydroxyapatite. The formation of this layer allows bioactive glass to bond firmly with both hard and soft tissues. Furthermore, bioactive glass can be manufactured to release nutrients required for bone regeneration.
It has been shown that damaged bone regained its original strength more quickly when repaired using composite combined with bioactive glass compared with bone repair using composite alone and that the efficacy achieved is comparable to that of autologous bone grafting.10,11
A recent study compared spine fusion in rabbits using a mineralized collagen bone substitute with and without added bioactive glass. The bioactive glass-collagen composite was shown to closely mirror repair by autograft in terms of the amount and quality of the new bone.12 In addition, fusion occurred earlier when the collagen composite was augmented with bioactive glass.13
Conclusion
Bone grafting is an important tool for the repair of damaged or disease bone. The gold standard is autografting, which uses bone harvested from the patient to avoid rejection reactions. However, the increased morbidity caused by the additional surgery needed to acquire bone for grafting has resulted in an on-going quest to find an alternative. Bone substitutes have shown efficacy, but do not promote the formation of new bone. Bioactive glass is biocompatible and enhances strong new bone creation. Studies have now shown that the addition of bioactive glass to bone substitutes can increase their efficacy and bone healing characteristics to rival those achieved with autografting.
Mo-Sci produces medical implant grade bioactive glass in a form suitable for mixing with bone composites and can tailor its composition to meet specific requirements.13
References
- Kinaci A, et al. Trends in Bone Graft Use in the United States. Orthopedics 2014;37(9):e783 e788.
- Flierl MA, Outcomes and complication rates of different bone grafting modalities in long bone fracture nonunions: a retrospective cohort study in 182 patients. J Orthop Surg Res. 2013;8:33.
- Rahaman MN, et al. Bioactive glass in tissue engineering. Acta Biomaterialia 2011;7:2355 2373.
- Bajammal SS, et al. The use of calcium phosphate bone cement in fracture treatment: a meta-analysis of randomized trials. J Bone Joint Surg [Am] 2008;90-A:1186-1196.
- Swiontkowski MF, et al. Recombinant human bone morphogenetic protein-2 in open tibial fractures: a subgroup analysis of data combined from two prospective randomized studies. J Bone Joint Surg [Am] 2006;88-A:1258 1265.
- Lerner T, et al. A level-1 pilot study to evaluate of ultraporous beta-tricalcium phosphate as a graft extender in the posterior correction of adolescent idiopathic scoliosis. Eur Spine J 2009;18:170-9.
- Dimar JR, et al. Clinical and radiographic analysis of an optimized rhBMP-2 formulation as an autograft replacement in posterolateral lumbar spine arthrodesis. J Bone Joint Surg [Am] 2009;91-A:137 186.
- Carragee EJ, et al. A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. Spine J 2011;11:471 191.
- American Academy of Orthopaedic Surgeons. Bone-grafts: Facts Fictions and Applications. Presented at 70th Annual General Meeting. Louisiana 2003. Available at https://www.aaos.org/research/committee/biologic/bi_se_2003-1.pdf
- Havener MB, et al. Improvements in Healing with a Bioactive Bone Graft Substitute in a Canine Metaphyseal Defect. Poster at 55th Annual Meeting of the Orthopaedic Research Society. February 22–25, 2009
- Jia W, et al. Bioactive Glass for Large Bone Repair. Adv Health Mater. 2015;4(18):2842 2848.
- Pugely AJ, et al. Influence of 45S5 Bioactive Glass in A Standard Calcium Phosphate Collagen Bone Graft Substitute on the Posterolateral Fusion of Rabbit Spine. Iowa Orthop J. 2017; 37: 193–198.
- Mo Sci Corporation website. http://www.mo-sci.com/en/products