Using Bioactive Glass to Encourage Implant Fixation
Posted on Jan 5, 2018
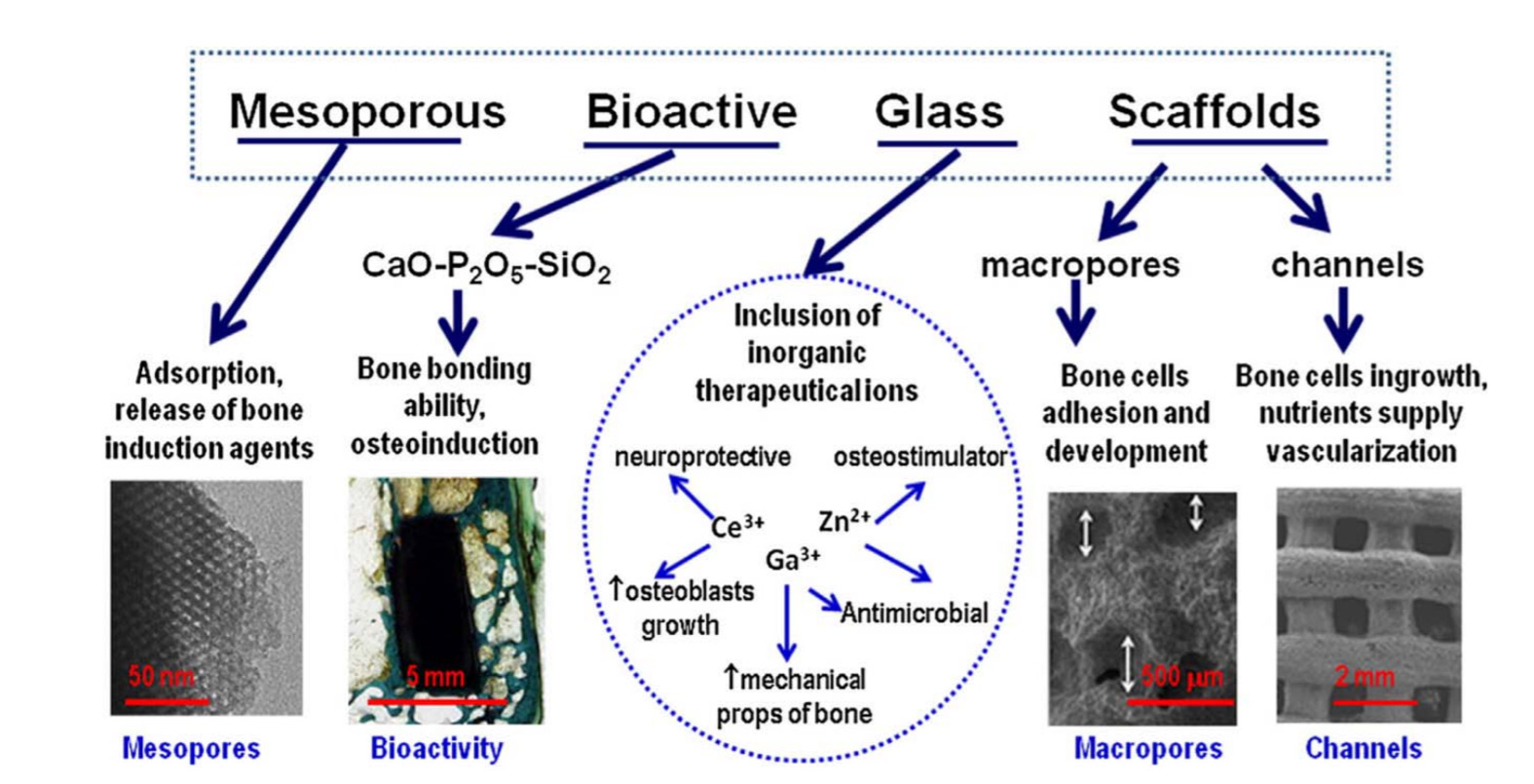
Bioactive glass induces specific biological activity when implanted in the body that causes the glass to become covered with a substance similar to hydroxyapatite. The formation of this layer allows bioactive glass to bond firmly with both hard and soft tissues.
This behavior has instigated extensive research into the use of bioactive glass to facilitate the repair of damaged bone. Furthermore, these bioactive glasses are biocompatible, and so do not elicit immune responses that can lead to rejection of foreign materials introduced into the human body.
Although brittle, bioactive glass offers a strong, yet lightweight, biodegradable framework to support healing. Furthermore, new borate and borosilicate bioactive glasses have been shown to enhance bone regeneration. In addition, the composition of bioactive glass can be adjusted to determine how long it persists in the body before it degrades so it provides support as long as is needed.1
Considerable success has been achieved using bioactive glass in the repair of bone, soft tissue and cartilage.1 Bioactive glass has also been shown to be beneficial in periodontal reconstruction2 and to promote the healing of ulcers in patients at risk of leg amputation.3
The efficacy of bioactive glass in enhancing the healing of both hard and soft tissues led to investigation into their application in reconstructive surgery requiring the use of permanent implants. This article explores how bioactive glass can help encourage the integration of implants.
Ensuring that Implants are Biocompatible
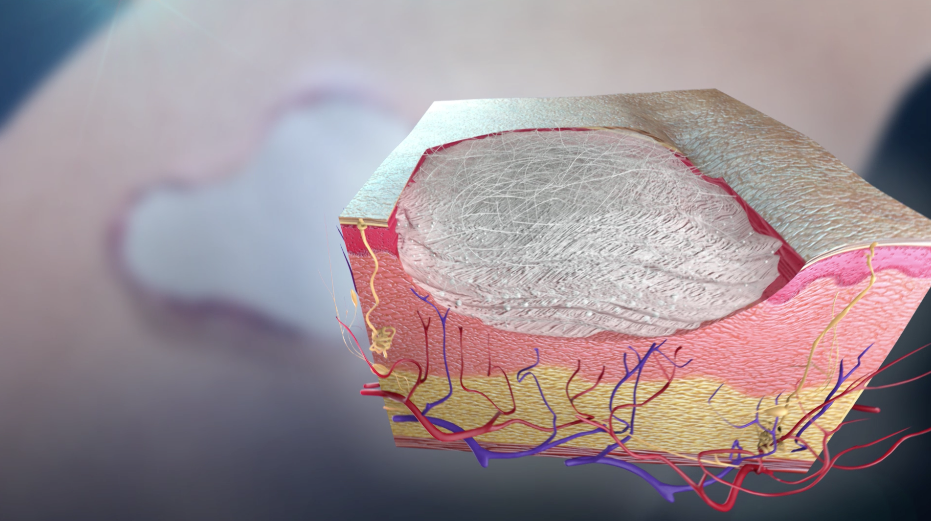
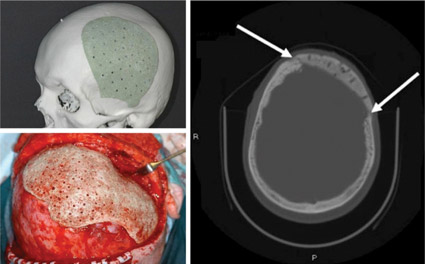
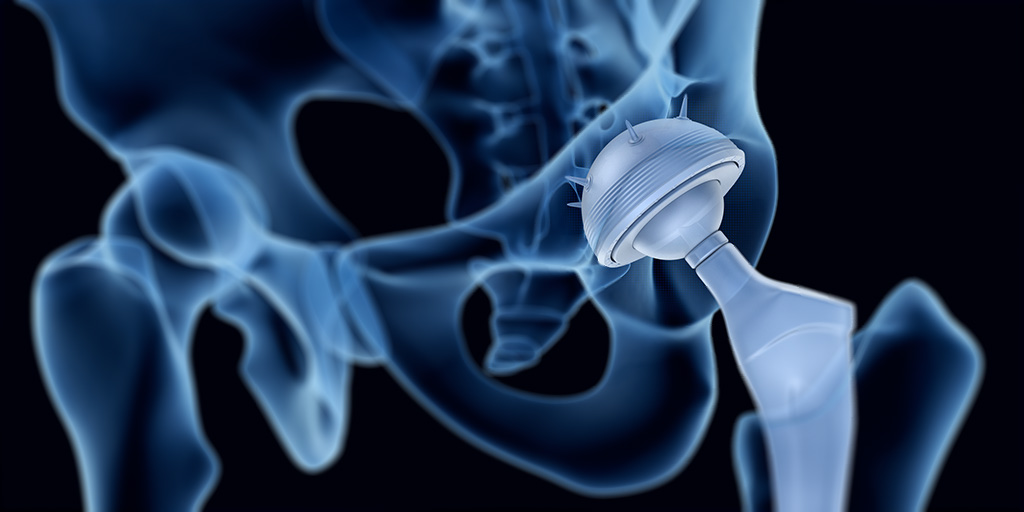
The human body has an amazing capacity to heal itself. However, in the case of multiple or complex fractures or serious infection or disease there can be too much of the original bone missing for it to heal satisfactorily. In such cases a bone graft or scaffold is required to support regeneration or bone fusion. Similarly implanted devices, such as plates, or screws and joint replacements, may be needed to reinforce or replace weak or damaged bones and joints. Similarly, implants may be required in dentistry to facilitate artificial replacement of a tooth root. These are usually in the form of a metallic screw positioned in the jaw bone that can support one or more false teeth.
Bone taken from another part of the patient’s body, an autograft, is the preferred implant for bone repair since it will not be at risk of rejection. However, this can be hampered by availability or suitability and incurs additional morbidity for the patient at the site from which the graft is harvested.
Titanium alloy implants have good biological compatibility but, in order for the implant to provide a strong structural support, it must be integrated into the bone (osseointegration) and it can take several months for the bone to grow in and/or around the implant. The implant must also be mechanically and morphologically compatible so it maintains good contact with the recipient bone to promote bony cell growth. In addition, there is the risk of metal implants being corroded by body fluids and releasing potentially toxic products.
Consequently, there has been much research into coatings for prosthetic metallic implants.4
Coating Implants in Bioactive Glass
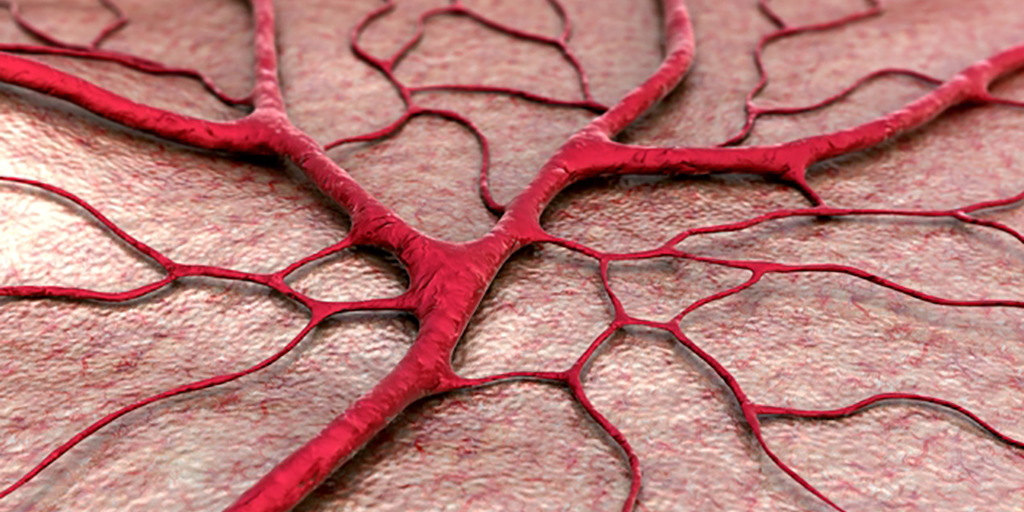
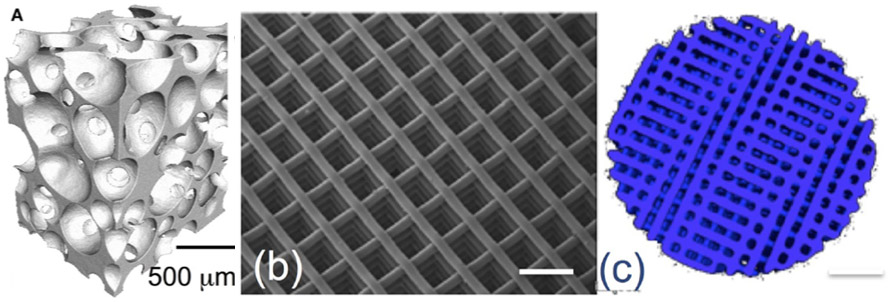
Bioactive glass is one such coating material that is currently the focus of much research. Once in the body, an amorphous calcium phosphate layer forms on the surface of bioactive glass. Within hours, this layer incorporates blood proteins and collagen and crystallizes into hydroxycarbonate apatite. This layer is now very similar to natural bone mineral, and so bonds readily to the recipient tissues/bone. Bioactive glass is therefore a prime candidate for coating implants that need to become integrated into bone.
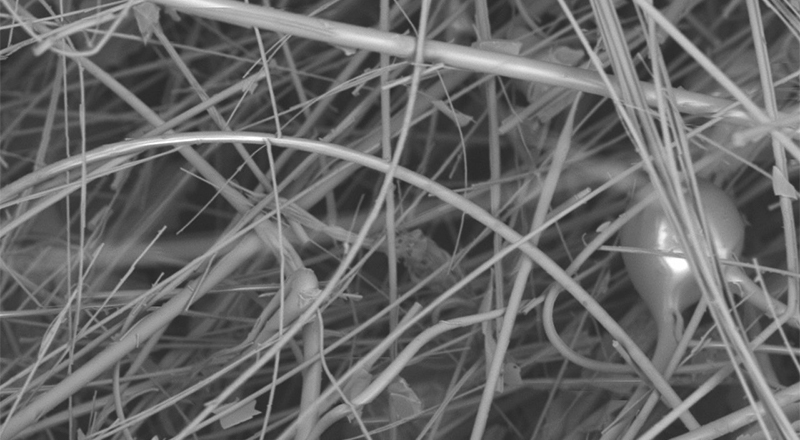
Including bioactive glass in polymeric scaffolding materials has been shown to accelerate the formation of a strong bond between the scaffold and tissue and promote healing.5 It followed that similar technologies may facilitate the osseointegration of the implants.
Numerous technical challenges have been overcome and titanium implants have been successfully coated with bioactive glass4 and evaluations of bioactive glass-coated implants have had promising results.6,7,8 Bioactive glass coatings on both orthopaedic and dental implants were shown not induce any adverse effects or inflammatory response in the surrounding tissue6. Furthermore, bioactive glass coatings accelerated cell attachment, spreading, proliferation, differentiation, and mineralization of the extracellular matrix and promoted rapid bone growth.6,7 In addition, the proportion of bone-to-implant contact were significantly greater for implants coated with bioactive glass.8
Bioactive glass can be obtained in a range of sizes and compositions9 suited to a range of applications. Indeed, bioactive glass can be custom made to specifications that precisely match a specific need, in terms of strength, degradation rate etc.
Conclusion
Implants are commonly needed in orthopaedic surgery to facilitate the repair of damaged or missing bone and in dental reconstructions. Although implants have been used with great success, procedures may be limited by rejection issues and toxicity concerns. Furthermore, it can take several months for an implant to become integrated into the recipient bone and this increases the risk of failure and prolongs recovery times.
The biocompatibility and strength of bioactive glass along with its ability to promote tissue regeneration has made it an invaluable tool in tissue engineering. With recent technological advances, it is now possible to coat metal implants with bioactive glass. Implants coated in this way have demonstrated great advantages in terms of both patient safety and recovery. The bioactive glass coating protects the metal implant from corrosion by bodily fluids thereby minimizing the risk of potentially toxic products entering the body. It also promotes new bone growth so the implant becomes secured in the bone more rapidly.
Bioactive glass coatings on implants can be used to encourage implant fixation, improve healing rates and maximize implant effectiveness.
Mo-Sci produce high quality bioactive glass in a form suitable for coating implants and can tailor its composition to meet specific requirements.
References
- Rahaman MN, et al. Bioactive glass in tissue engineering. Acta Biomaterialia 2011;7:2355 2373.
- Sohrabi K, et al. An evaluation of bioactive glass in the treatment of periodontal defects: a meta-analysis of randomized controlled clinical trials. J Periodontol 2012; 83: 453 464.
- The American Ceramic Society Press release 4 May 2011. Available at https://www.sciencedaily.com/releases/2011/05/110503133056.htm
- Lopez-Esteban S, et al. Bioactive glass coatings for orthopedic metallic implants. Journal of the European Ceramic Society 2003;23:2921–2930.
- Lu HH, et al. Three-dimensional, bioactive, biodegradable, polymer-bioactive glass composite scaffolds with improved mechanical properties support collagen synthesis and mineralization of human osteoblast-like cells in vitro. J Biomed Mater Res 2003;64A:465–474.
- Mehdikhani-Nahrkhalaji M, et al. Biodegradable nanocomposite coatings accelerate bone healing: In vivo evaluation. Dent Res J (Isfahan). 2015;12(1):89 99.
- Chen Q, et al.Cellulose Nanocrystals–Bioactive Glass Hybrid Coating as Bone Substitutes by Electrophoretic Co-deposition: In Situ Control of Mineralization of Bioactive Glass and Enhancement of Osteoblastic Performance. ACS Appl Mater Interfaces. 2015 Nov 11;7(44):24715 25.
- van Oirschot BA, et al. Comparison of different surface modifications for titanium implants installed into the goat iliac crest. Clin Oral Implants Res. 2016;27(2):e57 67.
- Mo Sci Corporation website. http://www.mo-sci.com/en/products